
UCSF researchers develop first-of-its-kind measure of gait performance, allowing researchers to fine tune electrical pulses to the neural network.
For patients with Parkinson's disease, changes in their ability to walk can be dramatic. “Parkinson’s gait,” as it is often called, can include changes in step length and asymmetry between legs. This gait dysfunction reduces a person’s mobility, increases fall risk, and significantly impacts a patient’s quality of life.
While high-frequency deep brain stimulation (DBS) is highly effective for lessening symptoms of tremors, rigidity, and bradykinesia, its impact on gait has been more variable and less predictable among patients with advanced gait-related problems. Significant challenges in enhancing DBS outcomes for advanced gait disorders have included the lack of a standardized gait metric for clinicians to use during programming, as well as understanding the impact of different stimulation factors on gait.
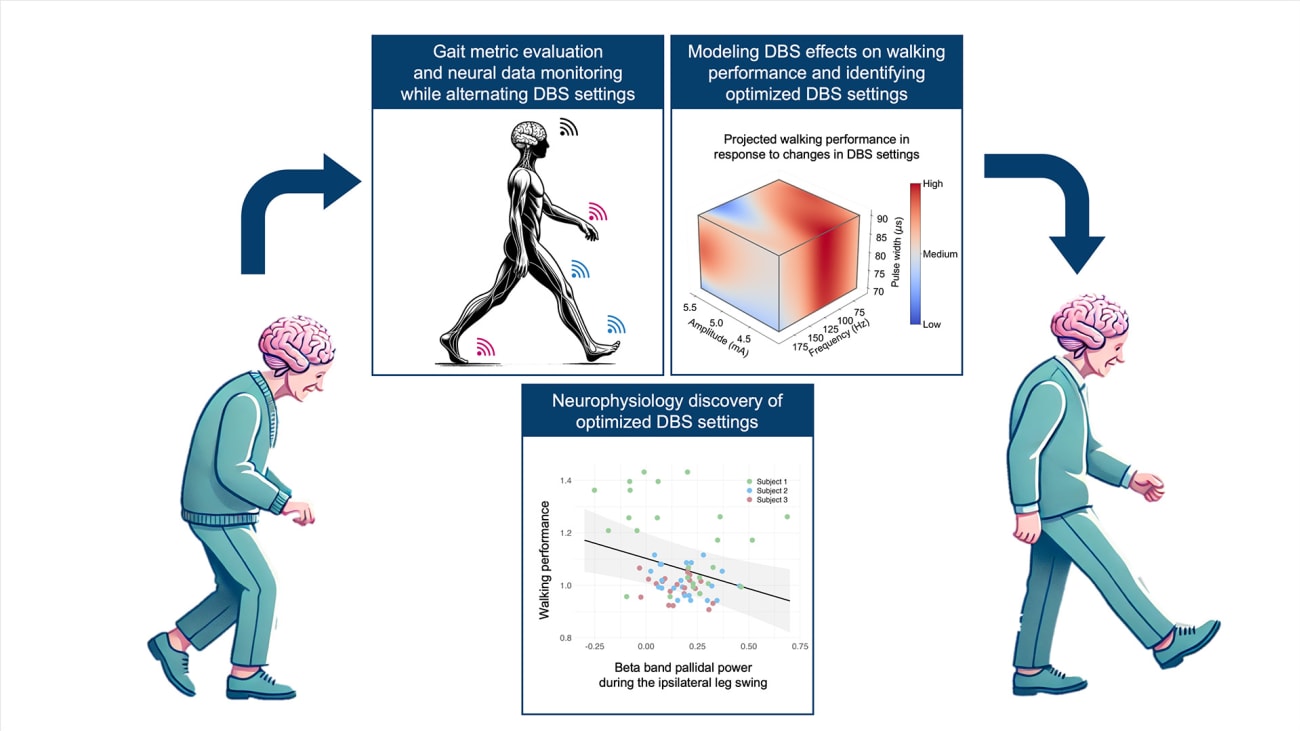
In a new study, researchers at UCSF developed a systematic way to quantify key aspects of gait relevant to Parkinson’s and used machine learning to identify the best DBS settings for each individual. These personalized settings led to meaningful improvements in walking, such as faster and more stable steps, without worsening other symptoms.
Their study results were published June 18, in the Nature publication, npj Parkinson’s Disease.
“We approached the problem of optimizing DBS settings as an engineering challenge, aiming to model the relationship between stimulation parameters, brain activity, and walking performance,” said study first author Hamid Fekri Azgomi, PhD, a postdoctoral scholar in the Wang Lab at UCSF.
How to optimize gait performance
In the study, patients with Parkinson’s were implanted with a DBS device that both stimulates the brain and records neural activity during walking. During clinic visits, patients’ DBS settings were altered within safety ranges to examine their impacts on gait functions. In response to each set of DBS settings, participants walked in a loop of approximately six meters with continuous streaming of their neural data and gait kinematics.
The researchers then developed and utilized a walking performance index (WPI) to assess gait metrics such as step length, stride velocity, and arm swing amplitude, to provide insight into gait consistency. By combining these metrics, the WPI offered a comprehensive assessment of gait, addressing multiple dimensions of motor function affected by Parkinson’s disease.
“Our results confirmed that changes in DBS settings were effectively captured by the WPI, aligning with patient and clinician evaluations during each visit,” said Azgomi. “This validation supports that the WPI is an effective metric for assessing and targeting gait improvements in people with Parkinson’s. Using these techniques, we were able to predict and identify personalized DBS settings that improved the WPI.”
First, the researchers identified brain activity patterns linked to better walking. By using multivariate models, the authors then identified distinct neural dynamics that differentiate optimal gait performance from less effective patterns. Improved gait correlated with reduced beta-band brainwave activity during specific phases of the gait cycle in the globus pallidus, which is a part of the brain associated with a loss of muscle movement in people with Parkinson’s.
These findings, along with identified person-specific neural biomarkers, underscore the importance of personalized, data-driven interventions for gait enhancement for people living with Parkinson’s.
“This work not only deepens our understanding of how DBS affects movement but also highlights the promise of personalized neuromodulation for Parkinson’s and other neurological disorders, bringing us closer to smarter and more effective neuromodulation therapies,” said senior study author Doris Wang, MD, PhD, a neurosurgeon and UCSF associate professor of Neurological Surgery.
The authors say that future directions for this research include developing automated systems for real-time gait analysis and integrating WPI with DBS programming software. Technologies such as gait mats, wearable sensors, and advanced motion capture systems could enable continuous and precise monitoring of gait, allowing for more accurate DBS adjustments.
Additional UCSF Authors: Kenneth H. Louie, PhD, Jessica E. Bath, DPT, PhD, Kara N. Presbrey, PhD, Jannine P. Balakid, BS, Jacob H. Marks, BA, Thomas A. Wozny, MD, Nicholas B. Galifianakis, MD, Marta San Luciano, MD, Simon Little, MBBS, Philip A. Starr, MD, PhD.
Funding: This study is supported in part by NIH grant R01NS130183 (R01), MJFF grant MJFF-010435 (MJFF), and the Burroughs Wellcome Fund Career Award for Medical Scientists.
Disclosures: Doris Wang consults for Medtronic, Boston Scientific Corp. ((unrelated to the content of this manuscript) Philip Starr receives support from Medtronic and Boston Scientific for fellowship education (unrelated to the content of this manuscript). Simon Little consults for Iota Biosciences (unrelated to the content of this manuscript).
About UCSF Health: UCSF Health is recognized worldwide for its innovative patient care, reflecting the latest medical knowledge, advanced technologies and pioneering research. It includes the flagship UCSF Medical Center, which is a top-ranked specialty hospital, as well as UCSF Benioff Children’s Hospitals, with campuses in San Francisco and Oakland; Langley Porter Psychiatric Hospital and Clinics; UCSF Benioff Children’s Physicians; and the UCSF Faculty Practice. These hospitals serve as the academic medical center of the University of California, San Francisco, which is world-renowned for its graduate-level health sciences education and biomedical research. UCSF Health has affiliations with hospitals and health organizations throughout the Bay Area. Visit http://www.ucsfhealth.org/. Follow UCSF Health on Facebook or on Threads.


