A team of UCSF surgeons devised a successful reconstruction approach during a complex Whipple procedure in a 69-year-old man with locally advanced pancreatic adenocarcinoma. While life expectancy for this condition is typically nine to 11 months, the patient continues to enjoy a good quality of life more than a year after diagnosis.
“We have removed a lot of these locally advanced tumors. We’re pushing the envelope,” said Carlos Corvera, MD, chief of the UCSF Hepatobiliary and Pancreatic Surgery Program and a member of the patient’s surgical team.
Neoadjuvant therapy shrank tumor
Computed tomography (CT) imaging of the patient’s tumor before chemotherapy and radiation showed it surrounding the portal vein and superior mesenteric vein (SMV) confluence and abutting the superior mesenteric artery (SMA). Before moving forward with surgery, the team wanted a comfortable margin around the tumor.
The patient completed 12 cycles of chemotherapy and five doses of external beam radiation therapy. Chemotherapy shrank the tumor at the portal vein–SMV confluence, and radiation reduced its abutment on the SMA. The UCSF team tracked the patient’s CA 19-9 levels. After 12 cycles of chemotherapy, they decreased from above 4,500 units per milliliter to nearly normal.
Experienced team initiates unique reconstruction
The surgical team began with an approach similar to a pylorus-sparing Whipple procedure. After performing most of the dissection for the procedure, they observed the patient’s middle colic vein was involved in the tumor and had to be divided. They also noted an area of intense desmoplastic reaction surrounding the patient’s SMV. To expose the SMA and remove the tumor, they decided to divide the SMV.
“When we divided the SMV below the splenic vein I knew the inferior mesenteric vein (IMV) was open,” said UCSF transplant surgeon Ryutaro Hirose, MD, a member of the surgical team.
The team knew immediately that they had to ensure adequate blood supply to the bowel. Because of their surgical experience and extensive knowledge of anatomy, this highly specialized, multidisciplinary team was able to quickly adapt to the patient’s condition and initiate a unique reconstruction.
Vascular reconstruction for congestive mesenteric venous ischemia
Approximately 10 centimeters of the SMV were involved with the tumor. The team placed a polytetrafluoroethylene (PTFE) graft, and blood flow resumed. As PTFE grafts are prone to clotting when used during long operative times, the team repeatedly checked the graft, including through intraoperative ultrasound. The ultrasound showed poor flow, so the surgical team replaced the PTFE graft with a cryopreserved cadaveric vein conduit to restore flow from the SMV to the portal vein. The patient’s small bowel improved, but his right colon appeared to remain ischemic, so the team performed a right colectomy with a long Hartmann’s pouch and an end ileostomy.
Enteric reconstruction for reperfusion edema
After four cycles of perfusion and reperfusion, the patient’s bowels were edematous, though no longer appeared poorly perfused. The team noted that the stomach was not congested and had good collateral flow. “I determined the best plan was to plug the pancreas into the stomach,” Corvera said.
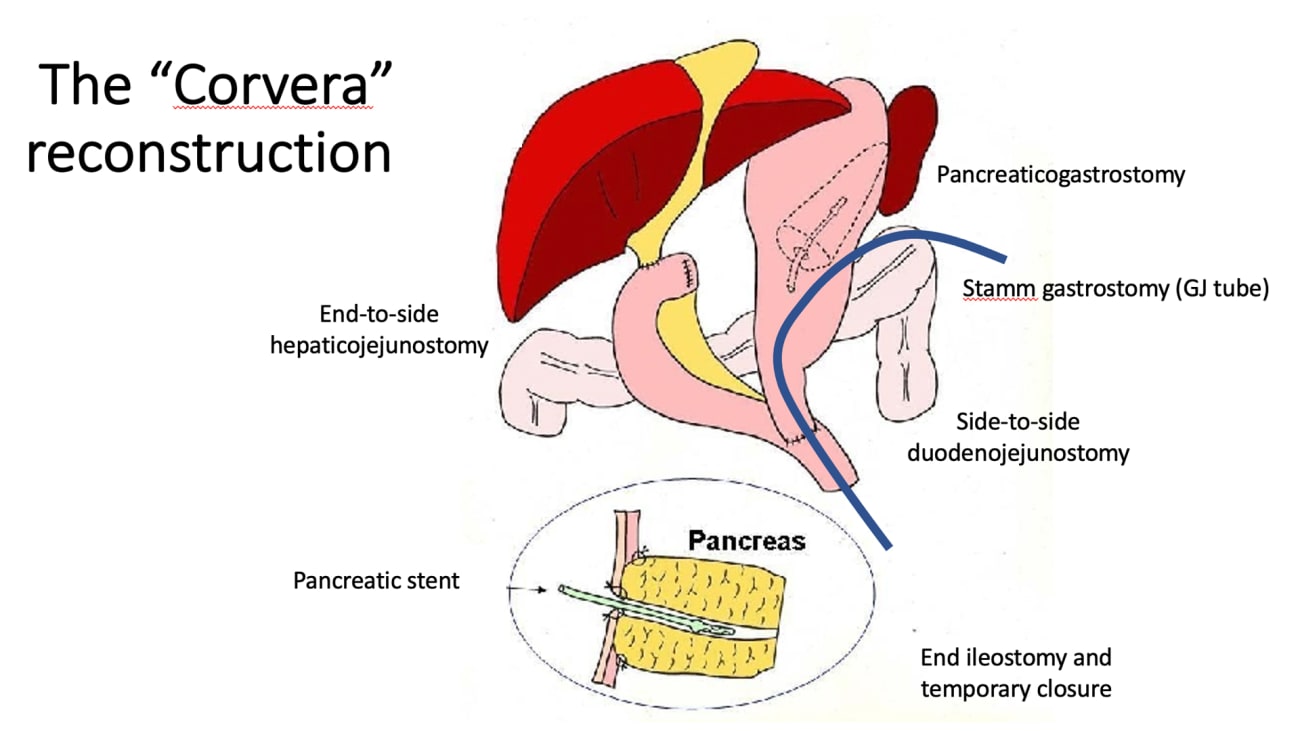
The UCSF team then performed a unique reconstruction. The first step was a pancreaticogastrostomy with a posterior and anterior gastrostomy; next was a side-to-side duodenojejunostomy. To address potential feeding difficulty for the patient and to vent the stomach, the team performed a Stamm gastrostomy with a gastrostomy-jejunostomy tube and finished with an end ileostomy. The only part of the classic Whipple used was an end-to-side hepaticojejunostomy. The team used a temporary closure, the best practice for this procedure.
“The venting gastrostomy was to decompress the bowel, which was massively dilated,” Corvera said. “With the venting ileostomy and decompression from above and below, everything worked really well.”
The patient was re-explored the next day, and perfusion to the entire remaining bowel looked pristine, so the patient was closed definitively. UCSF’s multidisciplinary surgical team of cancer, gastrointestinal and vascular experts made this complex, unique procedure possible.

Pre-treatment PET-CT

Post-surgical PET-CT
Good quality of life more than a year after diagnosis
The patient recovered well and was discharged 12 days after the procedure. The UCSF team achieved negative margins around the tumor, and the patient’s oncologist recommended no adjuvant chemotherapy. The patient’s CA 19-9 levels are checked every three months. He is able to enjoy food, activities and time with his family.
“Right now, he’s doing very well,” Corvera said. “Hopefully he’s going to continue to improve and have a good quality of life.”
Cancer research and treatment take place within the UCSF Helen Diller Family Comprehensive Cancer Center.
To learn more
UCSF Gastrointestinal Surgical Oncology Clinic
Phone: (415) 502-5577 | Fax: (415) 502-2236